Anecdote (not evidence?)
“The NHS is broken” Wes Streeting, Secretary of State for Health July 2024
A wise person once said, “the plural of anecdote is not evidence”. However sometimes anecdotes provide insight into where to look for evidence.
The following real-life patient stories illustrate the patient perspective – some good, some not so good and some things that need more thought.
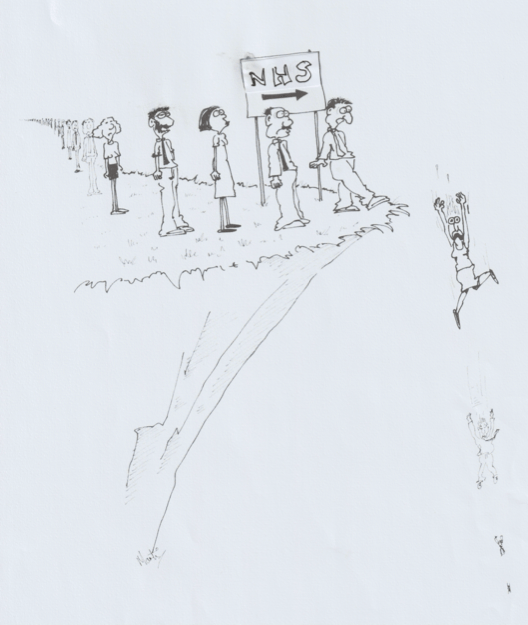
Diversions Take Longer
The thinking behind the introduction of other healthcare professionals into general practice is that patients can be treated by an appropriate person and GPs will be freed up to see more complex patients who really need to see a doctor.

It ignores the fact that patients are complicated, and their issues cannot always be parcelled into neat boxes.
MAPS in general practice: a better patient pathway?
There has been lots of coverage, in the mainstream media, and the medical media, about other health professionals seeing patients instead of doctors. They are a variety of people, called by different acronyms – MAPs (Medical Associate Professions) or AARS (Additional roles reimbursement scheme) in general practice.
A quick search on the internet will bring up lots of results about concerns from doctors about patient safety, the erosion of medical training and unemployed doctors. However very little can be found about what patients think about seeing ‘non-doctors’ apart from confusion and seeing several people before being sent back to their GP.
It was hoped that they improve access to general practice.
The new government is having a rethink.
MAPS Managing Long term conditions

Consulting with a clinical pharmacist (or other MAP) works very well when a long-term condition is stable. However, when things go downhill, it can be counterproductive when the treatment options offered are protocol driven because the clinician has a limited scope of practice.
NICE guidelines (and local guidelines) are just that – guidelines. But it seems that non-doctors use them as ‘must follow’ protocols. This is completely understandable. But what is not explained is the threshold for referring care of unstable LTCs back to a GP. The patient can be made to feel that they would be betraying trust if they went back to the GP to discuss other treatment options.
Patients need to know that a treatment pathway can go back to the GP when it becomes too complex for the MAP. This is not a failure of the MAP but just a recognition that LTCs are complicated and people with multiple co-morbidities sometimes do need to be treated by doctors.
Pause before sending
Some observations on text messages
Text messages are not new technology. General practice is now using text messages frequently as their computers allow them to send messages from the patient record. On the whole these messages don’t allow the patient to respond.
It’s great for appointment reminders, and other short messages. However, it is not a good substitute for a consultation, especially when it relates to a new diagnosis.
Case study:
Patient has been feeling excessively tired and achy for the past 4 months. She has put the symptoms to one side as her partner recently had life-changing surgery and she needed to focus on supporting him to get well.
He’s now on the mend and the patient finally got around to booking an appointment with her GP (for which she had to wait 4 weeks). The GP organised a raft of blood tests and booked a follow-up appointment for 2 weeks later.
The patient checked the NHS App for the results, but before they were posted she received a text message from another GP at the surgery:
Your thyroid function is very, very slightly out of range but the other markers of thyroid function are reassuringly normal. I do not think this is significant, but please book a repeat blood test in 6-12 weeks. Thank you.
The patient’s emotions were:
Relief – something that might explain the symptoms
Despair – having to potentially wait another 3 months of feeling awful until something would be done about it.
Irritation/Disappointment – Text messages, however reassuring in tone, should not be used to tell a patient about a potential new diagnosis. It gives no opportunity to ask about what the illness is, what treatment options there are, what is the prognosis, and how may it affect any other long-term conditions.
Asking someone who feels exhausted every day to wait another 3 months – without suggesting an opportunity for further discussion is not good care.
Eye emergency – by appointment only!
An eye-opening experience
There’s a lot of news everywhere about how the NHS is in crisis, and how people wait for ages to get an appointment with their GP. However, deep down we know that if we have something that is urgent our GP will see us on the same day. It may take a triage phone call, but they will try and fit us in if it’s urgent.
Call me naïve, but I thought the same thing would happen when I needed help with an eye problem.
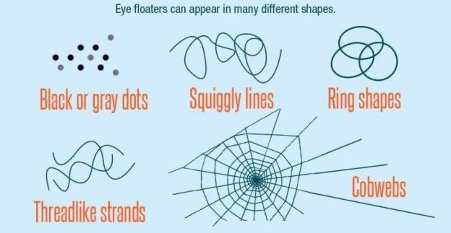
I was out walking when I felt as though I had a hair in my eye. I tried to brush it away but realised that there was nothing there. I then checked my glasses – they were also ok. It was like a spider hanging from a web moving around my eye. I called my optician to ask her advice. She told me to seek help urgently as it could be the first sign of a detached retina and directed me to the optician that provides the Oxfordshire Minor Eye Conditions Service (MECS). So, I walked there. They had no appointments for 3 days and suggested that I go to another optician. I then dropped into the optician next door. They were sympathetic and reiterated that I needed to be seen– but couldn’t help. They gave me the telephone number of the triage service at the Oxford Eye Hospital. Then I went to another optician. They also said that I needed to be seen but had no appointments available. They also commented that it was ‘late’ (3.30pm).
So, I called the Eye Hospital triage line. They agreed that I needed to be seen – but they closed at 4.30pm (by this time it was 4pm) so too late for that day. They made an appointment for the next morning. If things got worse overnight, I was instructed to go to A & E.
Long story short, I went to the eye hospital in the morning – they were very efficient, and I was in and out within 2 hours. Fortunately, it was not a detached retina (which would have required surgery).
The purpose of this story is that I was surprised at the difference in attitude between opticians, essentially private business, and general practice. On the one hand I was being told that this was a potentially urgent problem that needed to be checked without delay, but not one of the 4 opticians suggested that I come and wait, and they would ‘fit me in’. They were very sympathetic, but it was clear that none of them would see me without an appointment and because no appointments were available, I couldn’t be seen. So, I was pushed back into the main-stream NHS service. So much for more care in the community.